Hair transplant is the most effective solution for pattern hair loss. The FUSS or FUT technique (Follicular Unit Transplantation) or strip harvesting technique is a minimally invasive surgical procedure performed under local anaesthetic that can cover large areas with natural results.
The hair graft informative consult is essential for the correct indication of a micrograft as well as to inform patients of the realistic outcome expectations.
The consult on hair transplant consists of the following steps:
Although at first every patient can be a candidate for a hair transplant, it is important to observe the hair type of each patient, its placement, calibre and density; as well as the extension of the bald area that needs to be covered by the micrograft.
Two different scales are used to measure the suitability of micrograft hair replacement:
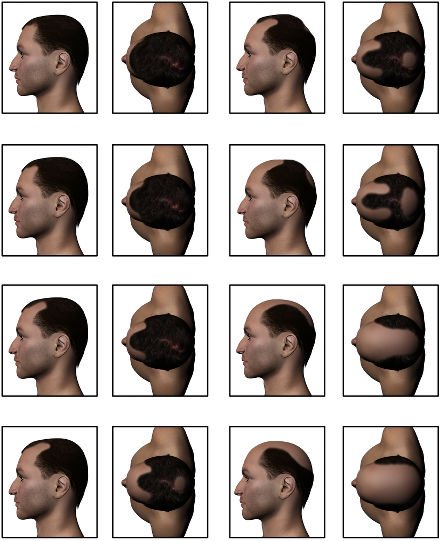
Norwood scale. Male hair loss classification
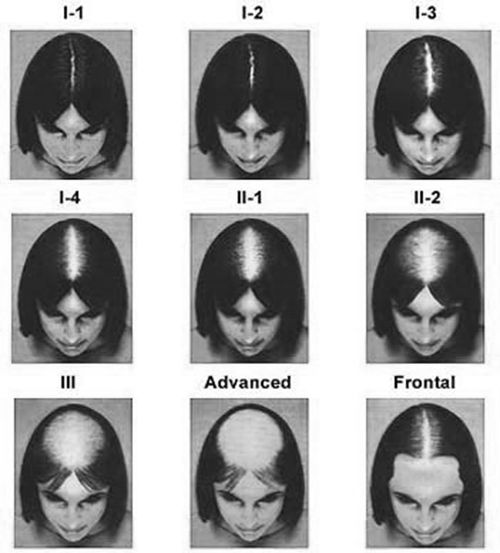
Ludwig scale: female hair loss classification
Hair thickness on the donor site is a conditioning factor in the degree of correction achieved in the final implant result. Hair thickness will create the sensation of density in the recipient site, more so than whether the transplanted follicles are fine and thin.
Hair density on the donor site will also determine the number of available follicles for grating as well as the final result. Most Caucasian patients have a density of 60 to 100 follicular units per square centimetre. Patients will less than 40 follicular units per square centimetre are inadequate for a transplant.
The extension in time and rate of the hair loss help us to establish and calibrate the advance and extension of baldness and loss of density.
Given the multifactorial nature of hair loss, it can never be ascertained precisely, but a fairly close approximation can de made.
As a general rule, patients with a loss of hair calibre at the end of adolescence or around age 20 are more likely to lose more hair and earlier than those who experience gradual thinning (atrophy), which is not cosmetically visible until the age of 30 or 40.
The degree of replacement achieved with a hair implant is conditioned by two factors:
For example, if a patient loses 1000 hairs over the course of a year and has 2000 hairs implanted, the final density reached will be 1000 hairs at the end of the first year and as time passes, the resulting density will be less. This is a clinical reality that the micrograft hair replacement patient must be aware of. They must know if the baldness can be considered stable or if it continues to evolve and may require additional hair transplant sessions.
The role of medication in hair transplant is an issue that should be discussed with the patient because it is of utmost importance to preserve pre-existing hair. Therefore, it is often recommended that the patient start a course of minoxidil or finasteride treatment to slow down hair loss.
In any case, when it comes to designing the micrograft hair replacement, the physician should plan in regard to the distribution of the hair. It must be considered that the patient may decide to quit the medication in the long-term and the area of existing hair can be cleared to a greater or lesser degree.
In addition, the physician must know any relevant details relating to the patient's health as well as the intake of medicines. Anticoagulant drugs greatly hinder this technique. In general, patients taking anticoagulant medication should request permission from their physician to suspend treatment for the hair implant procedure to be viable.
The hair transplant result must be natural throughout the years, regardless of whether the tendency for hair loss is maintained and the patient continues to progressively lose hair. This fact must be taken into consideration when defining the characteristics of the graft and must be discussed thoroughly with the patient.
In general, the front area of the scalp is the area where results are most assured and most visible for the hair graft, for both women and men. The crown is more difficult, because if the bald area continues to spread, the result can be unnatural over time, leaving an isolated micrograft in the centre of the crown, surrounded by a ring of complete baldness.

Before and after the hair transplant. Picture courtesy of Dr. Ruiz Alconero
The vast majority of hair grafts are performed with local anaesthetic. For patients with a high level of anxiety, a certain amount of sedation may be required.
Hair can be obtained by removing a strip of scalp (which is later broken down into small grafts consisting of one or several hairs) from the occipital region. Another method is the FUE technique, in which micrografts of 1 to 4 follicles are extracted and then directly grafted onto the recipient site.
Patients must be informed that if the hair is extracted from the donor site via the strip method, residual scarring can be somewhat visible if they decide to wear their hair very short or shaved. If the patient wears their hair short, the FUE technique is a better option.
Duration of the complete technique depends on the total number of micrografts to be transplanted. For 2,000 to 3,000 implants, the entire procedure could last 8 to 12 hours.
To improve patient comfort while undergoing micrograft hair replacement, they can listen to music, watch TV or films to keep them entertained. Once the technique is finished, the area may be bandaged or left uncovered. In either case, the patient must be careful not to injure the newly transplanted grafts.
In the days following the graft, 40 mg prednisone is prescribed for three days to reduce frontal oedema. Some physicians prescribe antibiotic prophylaxis and others advise only antibiotics the first day. Some patients require analgesic treatment the first few days and others have no discomfort. The patient should try to not make sudden movements during the first few days and ensure taking it easy during the first week.
After the first day, the patient can wash their scalp allowing the water to run gently without using shampoo or rubbing the area. On days 2 to 6, the patient can wash their head with baby shampoo (gentle) without scraping or rubbing using only their fingertips. On days 7 to 10, the stitches or staples are removed from the donor site in the case of strip harvesting. From this time on, the patient can resume their normal personal hygiene routine.
It is relatively difficult to predict the degree of future hair loss in young patients. While some patients at the age of 30 have evolved to VI degree on the Norwood scale, others just have slight, almost imperceptible atrophy that translates into a degree of thinning in the hair calibre.
In the first case, there may not be enough donor site to maintain a minimally acceptable hair density over time. Whereas in the second case, the patient might maintain and even recover part of the hair lost.
Commercially known as Propecia, it is taken orally and blocks the conversion of testosterone into dihydrotestosterone with the 5-alpha-reductase enzyme. Improvement in hair density and thickness is obtained 1 or 2 years after starting on the medication. Because it is absorbed by the blood, 2% of patients may experience decreased libido. The FDA has not authorised the use of finasteride for female alopecia, but it may improve when it is of androgenic origin. It is very important for women to know that finasteride should not be taken during pregnancy to avoid feminisation of a male foetus.
In the early days, it was used for the treatment of certain types of high blood pressure, then the impact it was having on androgenic alopecia was discovered and it was prescribed as a topical treatment in the format of a lotion against the hair loss. It is available in 2 to 5% solution and 5% gel formats. This medication must not be taken during pregnancy.
Whether associated or not to with a hair implant, patients who have this type of treatment must wait a minimum of 6 to 9 months to assess the partial result. The treatment must be carried out with perseverance and with a homogeneous dose to really assess the results.

Hair on the back of the scalp is not affected by male or female pattern baldness, so it becomes a reservoir of hair that serves as a donor site for the hair transplant.
In addition, the behaviour of hair extracted from this area retains its features despite being grafted to another location (frontal region), because it is genetically coded to survive and grow regardless of where it is finally located.
Thorough assessment of the quantity and quality of existing hair follicles in the area is essential, because these values have great weight in the successful outcome of the transplant.
In general, once the hair is harvested from the donor site there should be no signs of bald areas. In grafts harvested with the FUE technique, the 1 mm calibre marks made by the punch imperceptible. In the case of strip harvesting, a linear scar remains that can be imperceptible if sutured with a trichophytic closure. In any case, the patient should know that the incision area may be visible if hair is shaved or worn very short (less than 1 cm long).
Logically, the donor site is a very influential factor for the micrograft and has its limitations.
If the occipital area is genetically coded to lose some hair and thin out, this tendency will also occur in the hair follicles that are transplanted, and may partially alter the long-term result.
In cases where the occipital donor site has bald or scarred areas, the graft harvesting technique of choice is FUE. The patient should know that the total number of hair follicles that can be transplanted in one FUT (strip) session is normally higher than for FUE.
The donor site is usually located between the occipital protuberance and up to a virtual line that passes through the apex of the ears. Hair follicle density in the donor occipital area is typically 65 to 85 follicles per square centimetre. Hair follicle density will determine the size of the strip to remove in the case of FUT. In general, to ensure a good quality scar in the donor site for FUT (FUSS) grafts, it is recommended that the width of the strip does not exceed one centimetre. Preferably, the strip should be longer and narrower for an optimum final result in the donor site.

The donor site is anaesthetised with 1% lidocaine and 1:1,000,000 epinephrine along with a saline solution of 10 to 30 ml, depending on the preference of the surgeon to cause some turgidity in the tissue and facilitate the harvesting procedure.
The tumescent effect of the infiltration enables tissue manipulation, produces transient vasoconstriction that prevents bleeding and reduces the risk of transection in the case of FUE harvesting from the donor site. The best way to numb the anterior portion of the scalp is via anaesthetic ring block and truncal block of the supraorbital and supratrochlear nerves.
It is essential that harvesting is carried out at the appropriate depth. The incision must go beyond the follicle bulbs of the follicles in the subcutaneous cell tissue to prevent transections. In the case of strip harvesting, the donor site is closed with stitches or staple, which are removed 7-10 days later.
Trichophytic closure is a type of suture that camouflages the incision on the donor site for strip harvesting (FUT or FUSS).
The grafts are prepared by slicing the strip into small fragments of scalp containing 1 to 4 complete histological follicles for FUT (FUSS). The strip of scalp is separated into slices or layers and then each is broken down into small sections that contain 1 to 4 follicles. They are sorted by number of follicles and kept in a saline solution. Handling and preparation of the grafts in strip harvesting is a meticulous process that requires a microscope.
In the case of punch extraction (FUE technique), grafts are also harvested and kept in a saline solution then sorted by the number of hair follicles they contain. In this case, harvesting is significantly slower and there is a risk of injury to some of the follicles (transection), due to the extraction method.
It is very important to design the hair graft for a natural result. Some surgeons recommend using pre-defined distances for the delineation of the implant area taking into account certain anatomical relations.
One of the most important references is that the hairline must be about 8 or 9 cm from the glabella (between the brows).
Since the shape of patient heads are quite variable, the hairline design is different for each case and depends very much on the physician's training, their aesthetic and artistic sensibility.
One of the most important details when marking the area is to anticipate where hair loss will further progress and hair will be finer. Hair should not grafted beyond where the patient's previous hairline was (before the hair loss). Since the frontal hairline will gradually recede, it should be taken into consideration that the temporal line will also recede. Part of the temple area should be left hairless because the result is more natural.
In addition, the hairline must be irregular, slightly scalloped, to imitate the natural and spontaneous growth in that area. On the other hand, it is recommended that young patients do not receive grafts in the crown to prevent a bald ring forming around the area should the hair loss progress.
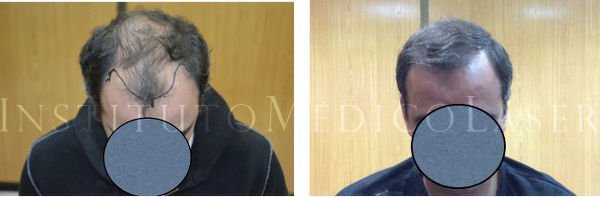
The initial design of the hair graft is important for natural results
Picture courtesy of Dr. Ruiz Alconero
The front hairline is central to a natural result, it is very important to frame the patient's face correctly. In the first graft, it is advisable to focus on the first third of the bald area, striving to respect pre-existing residual hairs. Therefore, magnifying glasses should be used during the implantation stage.
Patients with larger skulls may need more grafts to achieve the same cosmetic result as patients with smaller skulls. In both cases, it is very important to assess the density and quality of hair follicles from the donor site.
If additional hair grafts are implanted, we can work on the next mid third of the bald area towards the back. In any case, it is not recommended to transplant hair on the back area of the crown, because it is covered with the hair implanted on the front.
The location for grafts can be prepared using various tools, certainly the most frequent is the use of 18-20 G needles, with a calibre of 1.09 to 0.9 mm. The orifices can also be made with calibres under 0.7 or 0.6 mm.
It is very important that the holes are made at an angle of 30° to 60° and at a depth of 4 to 6 mm, going forward and behind the centre of the scalp to reproduce the hair's natural growth at an angle. The holes should be made with a light touch and not too close together, so as not to endanger graft survival. The ideal is to achieve a number of grafts per square centimetre of 20 to 35, which is 30 to 50% of the scalp's natural density. In patients with an excellent donor site, a graft density in the treated area of 40 - 50 grafts per square centimetre can be reached.
Special pliers are required to place the grafts in the orifices. The way in which the follicles are handled is essential to prevent compromising their vitality once transplanted. Cotton swabs are used for haemostasis and to prevent them from popping out. Popping occurs due to an increase in blood pressure, excess tumescent infiltration and the oedema resulting from the surgery. Depending on the quality of collagen in the recipient site scalp, there may be more tension and therefore more difficulty in retaining the grafts and increasing the incidence of popping.
Hair grows in small clusters of 1 to 4 grouped follicles. At the time when grafts were harvested with 3–4 mm punches, the grafts had 10 to 20 hairs and this provided an unnatural result. Nowadays, hair grafts are harvested with 1 mm punches or less. Therefore, there are 1 to 4 follicles in each graft and results are more natural and aesthetic.
Implanted hair usually enters the telogen stage, the hair shaft is dislodged and falls out. At 4-6 months, the new hair shaft emerges and grows with normal biological behaviour proper of its area of origin.
On occasion, the results of hair grafts carried out in the 1980s are cosmetically poor.
All hair grafts can be improved and artificial results corrected with corrective surgery or hair graft retouching.
When the follicles are grouped too close together, they can be partially fragmented by extraction with a punch then reinserted for a more natural effect.
If the patient wants to remove the implanted hair because they would rather return to their initial situation, laser hair removal can be performed. This can completely eliminate the hair, but sometimes does not remove the cobblestone effect that remains on the donor site.
Would you like to know if the FUT technique is suitable for you? Request a free informative consultation now with one of our expert surgeons from the IML Hair Transplant Unit.